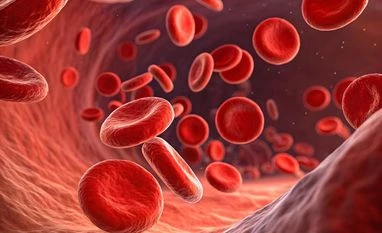
Globally, about 120 million blood units are donated each year, while demand stands at 220 million. In India, based on data up to 2022, the shortfall was around 1.5 million units a year. “This is the gap we’re trying to bridge — to help save more lives,” he says.
He points out that, like any pharmaceutical product, their blood will require regulatory approvals in both Israel and India, unlike donated blood, which faces fewer checks due to the lack of alternatives. At a price of $50 per unit, RedC’s product would be cost-competitive with donated blood, which must undergo pathogen testing — a step their in-lab process eliminates by design.
)